Radiology errors are sky rocketing. Radiologists are reading and reporting studies (aka films e.g. CT scans, MRIs etc) at an unprecedented pace. They are paid by the study not by the hour. It is a fact, the more studies a radiologist reads the more money they make, and ‘speed reading’ has become an unfortunate norm. The average CT of the head contains an excess of 800 individual images which is why radiology errors are increasing at an alarming rate.
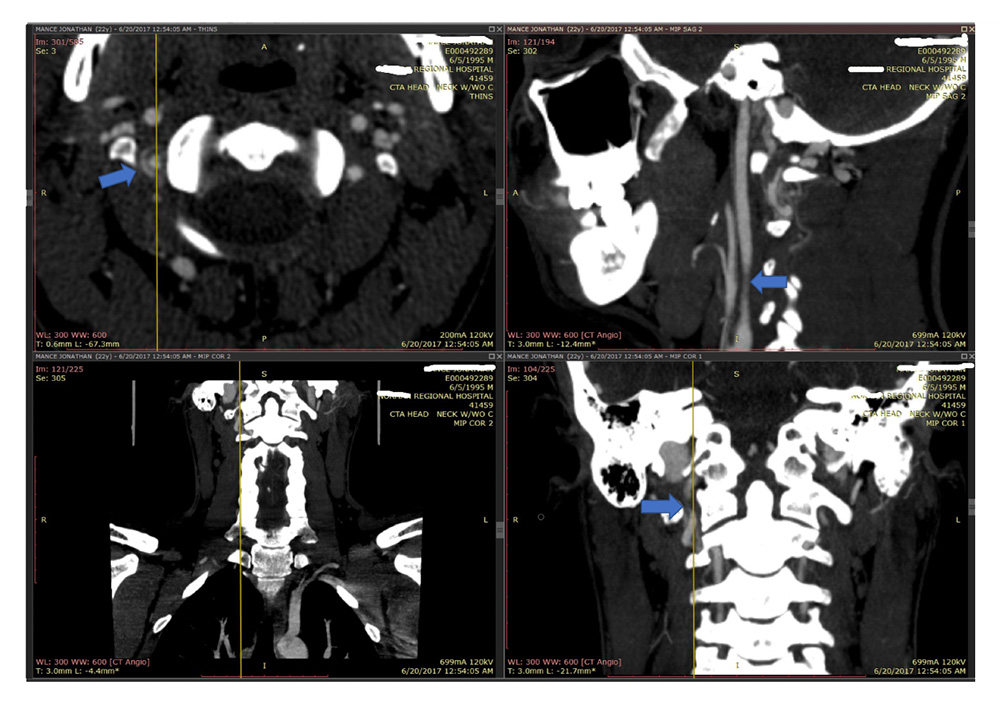
In one of my recent cases, a radiologist missed a critical vertebral artery dissection on a CT angiogram (images depicted). Several images on the CT angio study in multiple different planes clearly demonstrated the dissection, yet the radiologist missed it. Why? After investigation it was revealed that he ‘read’ over 1500 images in 87 seconds which is unconscionable. Why would a radiologist do this? Turn around times. Radiologists are racing the clock by corporate mandate. Hiring an experienced medical malpractice lawyer who understands this ‘corporatization of medicine’ can make the difference in the success of your case.
Radiology errors generally fall under one or more of the following categories:
Perceptual errors: when an abnormality is not identified.
- Under-reading: when the finding is not detected. It is the most common type of error.
- Lack of History: when a finding is missed because of an inaccurate, incomplete, or misleading clinical history.
- Lack of search: when a finding is missed because of failure to complete a systematic search after discovering an abnormality. It is the second most common type of error.
- Lack of proof reading the report: when a finding is missed because of over reliance on the radiology report from a previous examination.
- Location: when a finding is missed because it is outside of the area of interest.
- Image manipulation: when a radiologist fails to perceive an abnormality because of an inappropriate window (CT) or pulse sequence (MR).
Cognitive / interpretative errors: when an abnormality or a normal variant is seen but its meaning or importance is not correctly understood, resulting in an incorrect diagnosis.
- Complacency / Normal variant: when a clinically unimportant finding was appreciated but attributed to the wrong cause (false positive).
- Faulty reasoning: when the finding was appreciated and interpreted as abnormal, but attributed to the wrong cause (a true positive misclassified).
- Lack of knowledge: when the finding is correctly identified on the image, but its diagnostic importance is missed because of the reader’s lack of knowledge.
- Complication: when the finding missed is a complication from a procedure.
- Prior examination: when a finding is missed because of failure to consult prior studies or reports.
Communication errors: when the radiologist fails to effectively communicate the results including errors in the report, in making recommendations and in communicating important findings.
Technique or image acquisition errors: missed because of the technical or physical limitations of the imaging modality. Contributors to these types of errors include staff shortages, inexperience of the staff and inadequate equipment.
- Artifacts: imaging artifacts or technical factors might obscure the pathology due to image distortion (false negative) or might mimic pathology (false positive).
- Inappropriate study: when the indication of an image test is not correct, and the capability of a particular radiologic technique might not be suitable for the question that is being asked.
- Incomplete study: when the indication of an image test is correct, but does not include all the areas that must be studied.
https://www.carestream.com/blog/2017/05/15/increase-awareness-understanding-radiologic-error/

